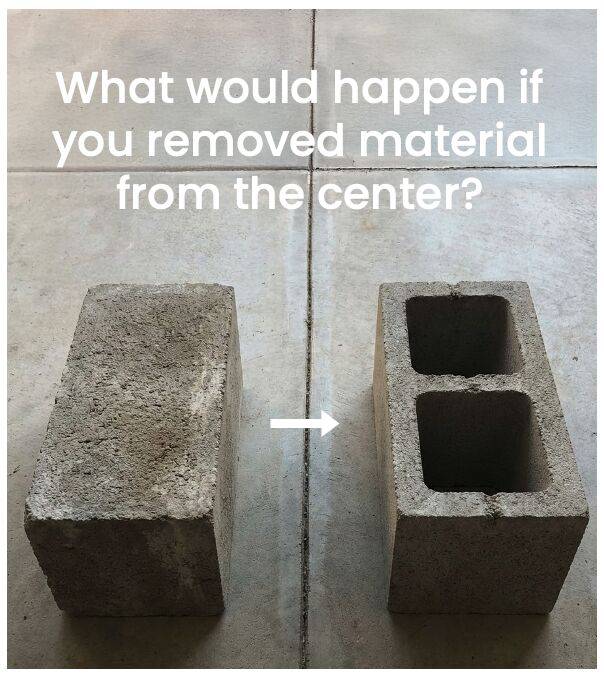
In 1890, inventor Harmon Palmer looked at a solid concrete block and asked a simple question: What would happen if you removed material from the center?
The result was a design that performed better in several ways. The hollow block was lighter and easier to handle, and the air trapped inside improved insulation, keeping buildings warmer in winter and cooler in summer. Most importantly, it remained strong where it needed to be strong.
That is the cinder block paradox: you can use less material and still get better performance at a lower cost.
U.S. healthcare needs the same kind of engineering mindset. We currently spend 18.5% of our GDP on healthcare, far more than other countries, yet our health outcomes lag significantly, ranking #48 in the world.
One of the biggest assumptions in healthcare is that lowering costs automatically means lowering quality. In other words, if we spend less, people must get worse care, and outcomes must decline.
But that tradeoff is far from inevitable. We have real examples where spending less can improve outcomes, as long as we remove the “mass” that isn’t doing any real work.
Consider a lesson from the high-cost drug management world. If physicians were to match real-world drug effectiveness data (from clinical trials and beyond) to patient-specific clinical and cost data, and we chose therapies based on the lowest true net cost instead of rebate-driven pricing games, we could reduce spending on high-cost drugs by 30% or more. In many cases, outcomes also improve because patients are now on the right drug at the right time, as per the data, rather than provider opinion.
The countries that outperform the U.S. didn’t get there by spending more across the board. They reduced wasteful, non-essential spending such as administrative complexity, opaque pricing, intermediary margins, and redundant processes that don’t improve health. At the same time, they invested more consistently in what drives better outcomes, including primary care, prevention, and care coordination.
A solid block is not necessarily stronger than a hollow one. It is just heavier.
Healthcare reform should not be framed as rationing. It should be framed as removing what does not carry value and reinforcing what does.
If we focus on that distinction, we can achieve better outcomes at a lower total cost.
Join us: https://tententen.org
HealthcareReform #HealthPolicy #HealthEconomics #ValueBasedCare #HealthcareInnovation #BetterOutcomes